What is Obsessive-Compulsive Disorder(OCD)?
Mental diseases are challenging. They are hard to diagnose, lack physical evidence (obviously) and are unique from one person to another.
Obsessive – Compulsive disorder is a mental illness that is very common in society and is on the rise. Obsessive-compulsive disorder (OCD) is a complex and debilitating mental health condition that affects individuals across various age groups and cultural backgrounds.
It is characterized by intrusive and distressing thoughts (obsessions) and repetitive behaviors or mental rituals (compulsions) aimed at reducing anxiety or preventing perceived harm.
OCD can significantly impair daily functioning, disrupt relationships, and cause immense distress. Understanding the nature, causes, and treatment of OCD is crucial in providing effective support and interventions for individuals affected by this challenging disorder.
This article aims to provide an overview of OCD, its diagnostic criteria, prevalence, etiology, and available treatment options, contributing to a comprehensive understanding of this condition and promoting improved mental health outcomes.
This post is all about obsessive – compulsive disorder, it’s symptoms, causes and potential treatment methods.
What is Obsessive Compulsive Disorder?
Obsessive-Compulsive Disorder (OCD) is a mental health condition characterized by the presence of obsessions and compulsions that significantly impact a person’s daily life. OCD affects people of all ages and is estimated to affect around 2-3% of the global population.
Obsessions in OCD are intrusive and unwanted thoughts, images, or urges that repeatedly enter a person’s mind. These obsessions are distressing and cause anxiety.
They often revolve around specific themes, such as contamination (fear of germs or dirt), symmetry and order (a need for things to be arranged perfectly), forbidden or taboo thoughts, or concerns about safety or harm. Individuals with OCD may experience intense anxiety, fear, guilt, or disgust associated with these obsessions.
Compulsions, on the other hand, are repetitive behaviors or mental acts that individuals with OCD feel compelled to perform in response to their obsessions. Compulsions are aimed at reducing distress or preventing a feared outcome.
Common compulsions include excessive cleaning or handwashing, checking behaviors (e.g., repeatedly checking locks or appliances), counting, arranging items symmetrically, repeating certain words or phrases silently, or seeking reassurance from others. Engaging in these compulsions may temporarily alleviate anxiety, but the relief is often short-lived, leading to a cycle of repetitive behaviors.
How Common Is OCD?

Obsessive-compulsive disorder (OCD) is a relatively common mental health condition that affects a significant number of individuals worldwide. Understanding the prevalence of OCD is essential for recognizing the impact it has on individuals and society. Here is an informative explanation of the prevalence of OCD:
Global Prevalence
OCD is recognized as one of the most prevalent mental disorders globally. The World Health Organization (WHO) estimates that approximately 2-3% of the world’s population will experience OCD during their lifetime. This means that tens of millions of individuals worldwide are affected by OCD.
Regional Variations
The prevalence of OCD may vary across different regions and countries. Studies have shown that cultural and societal factors can influence the expression and reporting of OCD symptoms. For example, research suggests that OCD is more prevalent in Western countries compared to non-Western countries.
However, it is important to note that these variations may be influenced by factors such as access to mental health services and cultural attitudes towards mental health.
Prevalence in Specific Populations
OCD can occur in people of all ages, including children, adolescents, and adults. Research indicates that the onset of OCD typically occurs during late adolescence or early adulthood. It is estimated that around 50% of individuals with OCD experience their first symptoms before the age of 18.
OCD affects both males and females equally, although certain subtypes of OCD, such as hoarding, may have a higher prevalence in specific populations.
Impact on Quality of Life
OCD is a chronic condition that significantly impacts the quality of life for individuals affected by it. The symptoms of OCD can be time-consuming, distressing, and interfere with daily functioning, relationships, and occupational activities.
It is associated with high rates of comorbidity, meaning that individuals with OCD often experience other mental health conditions such as anxiety disorders or depression, further exacerbating the burden of the disorder.
Importance of Seeking Help
Despite the high prevalence of OCD, many individuals with the disorder may not seek professional help or receive an accurate diagnosis. This may be due to stigma, lack of awareness, or a misconception that OCD is a personality quirk rather than a treatable mental health condition.
t is crucial for individuals experiencing symptoms of OCD to seek support from mental health professionals who can provide appropriate diagnosis, treatment, and support.
Understanding the prevalence of OCD helps raise awareness, reduce stigma, and promote early intervention.
If you or someone you know is experiencing symptoms consistent with OCD, it is advisable to consult a mental health professional for a comprehensive evaluation and appropriate treatment.
Early diagnosis and evidence-based interventions, such as cognitive-behavioral therapy (CBT) and medication, can significantly improve the well-being and functioning of individuals with OCD.
Related Article(s) – What is Tourettic OCD?
The OCD Cycle
The obsessive-compulsive cycle is a pattern of thoughts and behaviors that individuals with OCD experience. It involves a repetitive cycle of obsessions, anxiety, and the use of compulsions to alleviate the anxiety temporarily.
Here is an explanation of the obsessive-compulsive cycle along with a simplified graph illustrating the process:
Trigger/Stimulus
The cycle begins with a trigger or stimulus, which can be an external event, a thought, or an image. Triggers can vary depending on the individual’s specific obsessions. For example, a trigger could be touching a doorknob, having a disturbing thought about harm, or encountering a messy or disorganized environment.
Obsession
The trigger leads to the emergence of an obsession, which is an intrusive and distressing thought, image, or urge that enters the person’s mind. Obsessions are often irrational and inconsistent with the individual’s values, causing significant anxiety or discomfort. Examples of obsessions include a fear of contamination, concerns about safety, or a need for symmetry and order.
Anxiety
The obsession triggers a surge of anxiety or fear within the individual. The anxiety may stem from the perceived threat associated with the obsession or from the discomfort caused by the intrusive thought. The anxiety can be intense and overwhelming, further fueling the cycle.
Compulsion
To reduce or alleviate the anxiety caused by the obsession, the individual engages in compulsive behaviors or mental acts. Compulsions are repetitive actions or rituals that are performed in response to the obsession. They serve as a temporary relief from anxiety, providing a sense of control or a way to prevent a feared event. Common compulsions include excessive cleaning, checking, counting, arranging, or mental rituals like repeating phrases silently.
Temporary Relief
The compulsive behavior temporarily reduces the anxiety, giving the individual a brief sense of relief. This relief reinforces the belief that performing the compulsion is necessary to prevent harm or alleviate distress. However, the relief is short-lived, and the obsession resurfaces, restarting the cycle.
Increased Anxiety and Dependency
Over time, the obsessive-compulsive cycle strengthens. The individual may develop a dependence on compulsions as a coping mechanism, believing that engaging in these behaviors is necessary to prevent harm or alleviate anxiety. This can lead to an escalation of rituals and an intensification of anxiety associated with the obsessions.
Graph illustration of the obsessive-compulsive cycle:
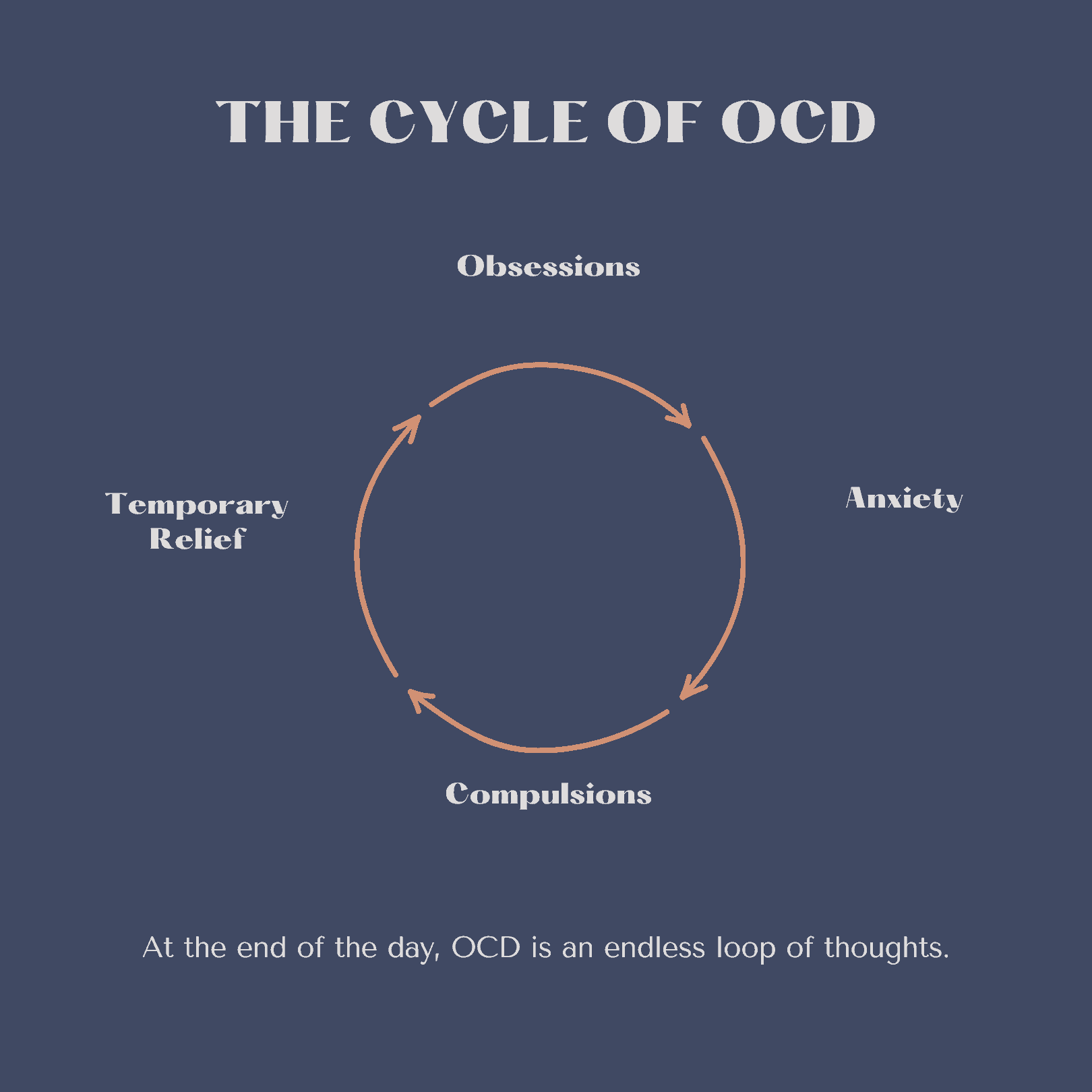
In the graph, the cycle starts with the trigger or stimulus, leading to obsessions, which then result in anxiety. The anxiety prompts the performance of compulsions, providing temporary relief. However, the relief is short-lived, and the cycle repeats itself over time, with the obsessions becoming more intense and the compulsions more elaborate.
Breaking the obsessive-compulsive cycle often involves therapeutic interventions such as cognitive-behavioral therapy (CBT) and exposure and response prevention (ERP). These approaches aim to help individuals challenge their obsessions, learn healthier coping strategies, and gradually reduce the reliance on compulsions to manage anxiety.
What are OCD Obsessions?
OCD obsessions are intrusive and persistent thoughts, images, or urges that individuals with obsessive-compulsive disorder experience. These obsessions are distressing and cause significant anxiety or discomfort. They often revolve around specific themes, and individuals with OCD may have one or more types of obsessions.
Here are several common types of OCD obsessions, along with detailed explanations:
Contamination Obsessions
These obsessions involve a fear of contamination or dirt. Individuals may be overly concerned about germs, bacteria, or toxins. They may worry that they will become ill or harm others if they come into contact with perceived contaminants. As a result, they may engage in excessive handwashing, avoidance of certain places or objects, or cleaning rituals to prevent contamination.
Symmetry and Order Obsessions
These obsessions revolve around the need for things to be “just right” or perfectly arranged. Individuals with this type of obsession may feel intense discomfort or anxiety when items are not organized symmetrically or if they are out of order. They may spend excessive amounts of time arranging objects, aligning items, or repeating certain actions until they feel a sense of balance or order.
Forbidden or Taboo Thoughts
These obsessions involve intrusive thoughts or images that are inconsistent with an individual’s values or beliefs. They may involve aggressive, sexual, or blasphemous content that the individual finds distressing. Despite the person’s understanding that these thoughts are irrational or unwanted, they can still cause significant anxiety. To alleviate the anxiety, individuals may engage in mental rituals or seek reassurance from others.
Harm Obsessions
These obsessions center around the fear of causing harm to oneself or others. Individuals may have intrusive thoughts of accidentally causing harm, being responsible for a tragic event, or intentionally hurting someone they care about. These thoughts can be distressing and lead to excessive checking behaviors, avoidance of certain situations, or seeking reassurance to prevent harm from occurring.
Related Article(s) – What is Harm OCD? Understanding Signs & Symptoms
Fear of Losing Control
This type of obsession involves a persistent fear of losing control of oneself, such as acting on violent impulses or behaving inappropriately. Individuals may worry that they will harm themselves or others, even though there is no evidence or likelihood of such actions. These obsessions can result in avoidance of certain situations, isolation, or constant mental checking and monitoring of one’s behavior.
Perfectionism Obsessions
These obsessions are characterized by an intense need for perfection in thoughts, actions, or performance. Individuals may experience anxiety and distress when they perceive that they have made a mistake or have not met their own high standards. They may engage in repetitive checking, reviewing, or revising behaviors to ensure perfection or prevent perceived errors.
It’s important to note that obsessions are typically unwanted and intrusive, causing distress and anxiety to individuals with OCD. They are not a reflection of a person’s true desires or intentions.
Obsessions can vary in intensity and frequency, and individuals may experience different combinations of obsessions. Understanding the specific types of obsessions an individual experiences is crucial in developing an appropriate treatment plan.
What Are OCD Compulsions?
OCD compulsions are repetitive behaviors or mental acts that individuals with obsessive-compulsive disorder engage in to alleviate the anxiety or distress caused by their obsessions. These compulsions are often performed in response to specific rules or rituals that the person believes will prevent harm, neutralize obsessions, or reduce anxiety temporarily.
Here are several common types of OCD compulsions:
Cleaning and Washing Compulsions
These compulsions involve excessive cleaning, washing, or sanitizing behaviors. Individuals may repeatedly wash their hands, take long showers, or clean surfaces excessively to rid themselves of perceived contamination. They may follow strict rituals or rules when performing these actions, such as a specific number of repetitions or using particular cleaning products.
Checking Compulsions
Checking compulsions involve repeatedly verifying or reassurance-seeking behaviors to alleviate fears or doubts. For example, individuals may repeatedly check locks, appliances, or electrical switches to ensure they are off or secure. They may review their work or repeatedly ask others for reassurance to confirm that a feared event did not occur.
Counting and Symmetry Compulsions
These compulsions revolve around repetitive counting or arranging behaviors. Individuals may feel compelled to count to a specific number or arrange objects symmetrically. They may repeat these actions until they feel a sense of “rightness” or balance, which temporarily reduces their anxiety.
Mental Rituals
Mental rituals are internal compulsions that individuals perform mentally to neutralize their obsessions or prevent harm. For example, they may silently repeat certain words or prayers, create mental images, or mentally review specific actions to counteract their intrusive thoughts or anxieties. These rituals can be time-consuming and may need to be repeated until the person feels temporary relief.
Ordering and Arranging Compulsions
These compulsions involve a strong need for order, symmetry, or exactness. Individuals may spend excessive amounts of time organizing objects or arranging items in a specific manner to achieve a sense of control or balance. They may become distressed if things are not arranged “correctly” and feel compelled to fix them repeatedly.
Related Article(s) – OCD Ordering And Arranging
Hoarding and Saving Compulsions
Some individuals with OCD exhibit hoarding behaviors or have difficulty discarding items. They may feel intense anxiety or distress at the thought of getting rid of possessions, even if they have no practical value. They may compulsively save items, collect excessive quantities of objects, or have difficulties organizing or decluttering their living spaces.
It is important to note that compulsions are intended to reduce anxiety temporarily and prevent feared outcomes associated with obsessions.
However, engaging in compulsions actually reinforces the cycle of OCD by maintaining the belief that the rituals are necessary. Over time, compulsions can become more time-consuming, intrusive, and disruptive to daily functioning.
Understanding the specific compulsions an individual engages in is essential in developing an appropriate treatment plan. Therapists work collaboratively with individuals to identify and modify these compulsions, helping them regain control over their lives and reduce the impact of OCD on their daily functioning.
What are Intrusive Thoughts In OCD?

Intrusive thoughts are a common symptom experienced by individuals with obsessive-compulsive disorder (OCD). They are involuntary, distressing, and unwanted thoughts, images, or impulses that repeatedly intrude into a person’s mind. These thoughts are often inconsistent with a person’s values, beliefs, or desires, causing significant anxiety, fear, or distress.
Here is a detailed and informative explanation of intrusive thoughts in OCD:
Characteristics of Intrusive Thoughts
Intrusive thoughts can manifest in various forms and themes, depending on the specific obsessions an individual has. They can be violent, sexual, aggressive, blasphemous, or related to contamination, harm, symmetry, or order. What distinguishes them is their intrusive nature, as they pop into the individual’s mind without deliberate control or invitation. Individuals with OCD typically find these thoughts distressing and recognize them as irrational or unwanted.
Prevalence of Intrusive Thoughts in OCD
Research suggests that intrusive thoughts are highly prevalent in individuals with OCD. A study by Rassin et al. (2001) found that 98% of individuals with OCD reported experiencing intrusive thoughts. These thoughts were found to be a significant source of distress and impairment in their daily lives.
Relationship with Obsessions
Intrusive thoughts are closely linked to the obsessions experienced by individuals with OCD. Obsessions are persistent and recurrent thoughts, impulses, or images that cause anxiety or distress. Intrusive thoughts often align with the content of obsessions and trigger the obsessional cycle. For example, a person with contamination obsessions may experience intrusive thoughts of being contaminated by harmful substances.
Appraisals and Misinterpretations
Individuals with OCD tend to interpret intrusive thoughts as highly significant and indicative of their true character or intentions. They may misinterpret the occurrence of intrusive thoughts as evidence of being dangerous, immoral, or prone to harmful actions. These misinterpretations contribute to the distress and anxiety associated with intrusive thoughts and reinforce the obsessional cycle.
Cognitive Biases
Cognitive models propose that individuals with OCD exhibit specific cognitive biases that contribute to the persistence and interpretation of intrusive thoughts. These biases include attentional biases, where individuals are hyper-focused on threat-related stimuli, and memory biases, where they recall more threatening or intrusive information. These biases contribute to heightened vigilance and the perception of increased threat associated with intrusive thoughts.
Treatment Approaches
Intrusive thoughts are targeted in cognitive-behavioral therapy (CBT) for OCD, specifically through exposure and response prevention (ERP). ERP aims to help individuals confront their fears and tolerate the distress associated with intrusive thoughts without engaging in compulsive behaviors or mental rituals. By gradually exposing individuals to the thoughts and preventing the associated compulsions, they learn to reduce the anxiety and distress triggered by the thoughts.
It’s crucial to understand that intrusive thoughts in OCD do not reflect an individual’s true character or desires. They are a symptom of the disorder and are not acted upon or willingly endorsed by the person experiencing them.
Seeking professional help from a qualified mental health professional, such as a therapist specializing in OCD, can provide appropriate diagnosis, support, and evidence-based treatment to address intrusive thoughts and their associated distress.
Enhance your knowledge of OCD and checkout our must read OCD books list!
What Are The Causes Of OCD?

The exact causes of obsessive-compulsive disorder (OCD) are not fully understood. However, research suggests that a combination of genetic, neurobiological, and environmental factors contribute to the development of OCD.
Here is a detailed and informative explanation of the potential causes of OCD:
Genetic Factors
There is evidence to suggest a genetic component in the development of OCD. Family and twin studies have shown that individuals with first-degree relatives (such as parents or siblings) with OCD have a higher risk of developing the disorder.
The heritability of OCD is estimated to be around 40-60%. Several genes have been implicated in OCD, including genes related to serotonin regulation, such as the SLC1A1 gene. However, no single gene has been identified as the sole cause of OCD.
Neurobiological Factors
Neurotransmitters, particularly serotonin, dopamine, and glutamate, play a role in the development and regulation of OCD symptoms. Dysfunction in the cortico-striato-thalamo-cortical (CSTC) circuit, which involves communication between different brain regions, is thought to contribute to the manifestation of OCD symptoms.
Neuroimaging studies have shown structural and functional abnormalities in brain regions such as the orbitofrontal cortex, anterior cingulate cortex, and basal ganglia in individuals with OCD.
Environmental Factors
Certain environmental factors may contribute to the development of OCD in susceptible individuals. These factors include childhood trauma, stressful life events, and infections, particularly streptococcal infections.
Research suggests that childhood adversity, such as abuse or neglect, may increase the risk of developing OCD later in life. In some cases, streptococcal infections can trigger the sudden onset or exacerbation of OCD symptoms, a condition known as pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS).
Cognitive Factors
Cognitive factors, such as maladaptive beliefs and cognitive biases, may contribute to the development and maintenance of OCD symptoms.
Individuals with OCD often have inflated beliefs regarding the importance of their intrusive thoughts and engage in excessive attempts to control or suppress these thoughts.
They may also exhibit cognitive biases, such as a heightened sense of responsibility, intolerance of uncertainty, and perfectionistic thinking, which can perpetuate the obsessions and compulsions.
It’s important to note that OCD is likely influenced by a complex interplay of multiple factors, and individual experiences may vary. Further research is needed to gain a comprehensive understanding of the causes of OCD.
If you or someone you know is struggling with OCD, seeking professional help from a mental health provider experienced in treating OCD is recommended for accurate diagnosis and appropriate treatment interventions.
Related Article(s) – What Causes OCD To Get Worse?
Advanced Treatment Methods In OCD

Cognitive-Behavioral Therapy (CBT):
CBT is typically delivered in a structured format and involves weekly sessions with a trained therapist.
Exposure and Response Prevention (ERP) is a key component of CBT for OCD. It involves gradually exposing individuals to situations, objects, or thoughts that trigger their obsessions.
During exposure, individuals are encouraged to resist engaging in their usual compulsive behaviors. This process helps them learn that their fears are unfounded and that they can tolerate the anxiety without resorting to compulsions.
Cognitive restructuring in CBT focuses on identifying and challenging irrational thoughts and beliefs associated with OCD. Through guided self-reflection and questioning, individuals learn to develop more rational and realistic interpretations of their obsessions.
Medication:
Selective Serotonin Reuptake Inhibitors (SSRIs) are the first-line medications for OCD. These medications increase the availability of serotonin in the brain, which helps regulate mood and anxiety. It may take several weeks for SSRIs to start showing their full therapeutic effects.
The dosage of SSRIs used for OCD is often higher than that used for depression. The specific SSRIs commonly prescribed for OCD include fluoxetine, fluvoxamine, sertraline, paroxetine, and escitalopram.
Clomipramine, a tricyclic antidepressant, is also approved for the treatment of OCD. It is generally considered when SSRIs are not effective or well-tolerated.
Augmentation Strategies:
If symptoms persist despite initial treatment, augmentation strategies may be employed. This involves combining different medications or adding medications from other classes to enhance treatment effectiveness.
Atypical antipsychotic medications, such as aripiprazole or risperidone, may be added to augment the response to SSRIs.
Benzodiazepines, such as clonazepam, may be used on a short-term basis to help manage acute anxiety symptoms, but they are generally not recommended as long-term treatments due to the risk of dependence.
Deep Brain Stimulation (DBS):
Deep brain stimulation is a surgical procedure that involves implanting electrodes in specific areas of the brain to modulate abnormal brain activity associated with OCD. It is typically considered for severe, treatment-resistant cases of OCD when other treatments have not been effective.
Self-Help Strategies:
Self-help strategies can support OCD treatment and promote overall well-being. These may include stress reduction techniques (e.g., deep breathing, mindfulness), regular exercise, maintaining a structured routine, engaging in pleasurable activities, and seeking support from friends, family, or support groups.
It’s important to remember that treatment for OCD should be individualized, and a combination of different approaches may be necessary.
Consulting with a mental health professional experienced in treating OCD is crucial for developing a personalized treatment plan that addresses the specific needs and challenges of each individual.
With effective treatment, many individuals with OCD can experience significant symptom reduction and improved quality of life.
Related Article(s) – What Will Happen if OCD is Left Untreated?
Final Thoughts OCD
In conclusion, obsessive-compulsive disorder (OCD) is a common and often debilitating mental health condition that affects individuals worldwide. It is characterized by intrusive and distressing thoughts (obsessions) and repetitive behaviors or mental rituals (compulsions). OCD can significantly impair daily functioning, relationships, and overall quality of life.
Fortunately, effective treatment options are available for OCD. The primary treatment approach is cognitive-behavioral therapy (CBT), specifically exposure and response prevention (ERP) and cognitive restructuring. ERP helps individuals confront their fears and resist engaging in compulsive behaviors, leading to a reduction in anxiety over time. Cognitive restructuring helps challenge and modify the maladaptive thoughts and beliefs that drive OCD symptoms.
Medication, particularly selective serotonin reuptake inhibitors (SSRIs), is often used in conjunction with therapy to alleviate symptoms of OCD. Augmentation strategies and other therapeutic approaches, such as acceptance and commitment therapy (ACT) and mindfulness-based interventions, may also be beneficial in certain cases.
It is important for individuals with OCD to seek professional help from mental health providers experienced in treating OCD. A comprehensive treatment plan should be tailored to the individual’s specific needs, involving a combination of therapy, medication, and self-help strategies. Early intervention and ongoing management can lead to significant improvements in symptom reduction, functional recovery, and overall well-being.
Moreover, increased awareness, understanding, and destigmatization of OCD are crucial in promoting early recognition and appropriate treatment seeking. Support from family, friends, and support groups can also play a vital role in the recovery process.
If you or someone you know is experiencing symptoms of OCD, reaching out to a mental health professional is recommended. With the right support and treatment, individuals with OCD can regain control of their lives, manage their symptoms, and lead fulfilling and productive lives.
This post was all about Obsessive – Compulsive Disorder, its symptoms, causes and potential treatment methods.




