Can Hormone Imbalance Cause OCD?

Curiosity often leads us to question the intricate relationship between our body’s hormonal balance and mental illness. One such query that piques interest is whether hormone imbalance can play a role in the development of Obsessive-Compulsive Disorder (OCD).
In this exploration, we embark on a journey to understand the potential connections between hormonal fluctuations and the onset of OCD symptoms and other anxiety disorders.
Join us as we navigate through this inquiry, seeking insights into the complex interplay between hormones and the intricate landscape of OCD.
Understanding OCD and Hormone Imbalance
Related Articles – 9 Overlooked Symptoms of OCD
Definition and Explanation of OCD
Obsessive-Compulsive Disorder (OCD) is a mental health condition characterized by persistent, intrusive thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed in response to these thoughts.
The obsessions and compulsions cause significant distress and interfere with daily functioning.
OCD is often considered a chronic disorder, but various treatments, including therapy and medications, can help manage symptoms.
Overview of Hormone Imbalance and Its Potential Effects on Mental Health
Hormone imbalance refers to disruptions in the normal levels of hormones in the body, impacting physiological functions.
Hormones, the body’s chemical messengers, play a pivotal role in regulating metabolism, growth, stress response, and reproductive functions.
Understanding how hormone imbalance may affect mental health involves examining specific hormonal components:
Stress Hormones (Cortisol)
Cortisol, released in response to stress, has profound implications for mental health.
Prolonged stress and elevated cortisol levels may contribute to anxiety disorders, including Obsessive Compulsive Disorder.
Dysregulation in the stress response system can amplify obsessive thoughts and compulsive behaviors.
Reproductive Hormones (Estrogen, Progesterone)
Fluctuations in reproductive cycle events, such as estrogen levels and progesterone levels, are associated with mood changes.
Hormonal shifts during the menstrual cycle, pregnancy, postpartum (postpartum OCD) or menopause may influence the severity of OCD symptoms.
The gender-specific nature of these influences underscores the need for tailored approaches such as hormone replacement therapy.
Thyroid Hormones
Thyroid hormones, vital for metabolism and cognitive function, can impact mental health.
Imbalances in thyroid hormones, whether hypothyroidism or hyperthyroidism, may contribute to cognitive difficulties and alterations in mood, affecting the cognitive dimensions of Obsessive Compulsive Disorder.
Neurotransmitter Regulation
Hormones regulate neurotransmitters, influencing brain function.
Serotonin, linked to OCD, is sensitive to hormonal changes.
Dysregulation in neurotransmitter systems can contribute to the neurobiological basis of OCD symptoms.
Lifespan Considerations
Hormonal changes during critical life stages, such as puberty, Postpartum OCD, pregnancy, and menopause, can coincide with the onset, exacerbation, or modulation of OCD symptoms.
Examining hormonal influences across the lifespan provides insights into the evolving nature of the relationship between hormones and OCD.
Environmental Influences
Beyond intrinsic factors, external elements in the environment can impact hormone levels and, consequently, OCD.
Stressors, lifestyle choices, and exposure to endocrine-disrupting substances may contribute to hormonal imbalances, highlighting the broader environmental context.
Implications for Assessment and Treatment
Recognizing the interplay between OCD and hormone imbalance informs assessment approaches, encouraging a comprehensive examination of hormonal profiles alongside traditional diagnostic criteria.
Treatment strategies may involve a nuanced combination of psychotherapy, pharmacotherapy, and lifestyle modifications, considering the specific hormonal dynamics contributing to individual experiences of OCD.
In essence, a detailed understanding of the intersection between OCD and hormone imbalance involves unraveling the intricate ways in which hormonal fluctuations such as postpartum obsessive compulsive disorder impact the cognitive, emotional, and neurobiological dimensions of the disorder including other psychiatric disorders and mental health issues.
The Impact of Hormones on OCD
Stress Hormones and OCD Intensity
Stress hormones, such as cortisol, not only respond to external stressors but also have a bidirectional relationship with OCD symptoms.
Elevated cortisol levels may heighten the sensitivity of the brain’s fear circuit, intensifying obsessive thoughts and compulsive behaviors.
Reproductive Hormones and Symptom Variation
Further exploration into the influence of reproductive events unveils a nuanced understanding of the hormonal landscape in OCD.
Hormonal shifts during the menstrual cycle, pregnancy, and menopause can trigger changes in serotonin levels, affecting mood and exacerbating OCD symptoms.
This knowledge prompts clinicians to consider hormonal fluctuations as potential contributors to symptom variation and tailor interventions accordingly.
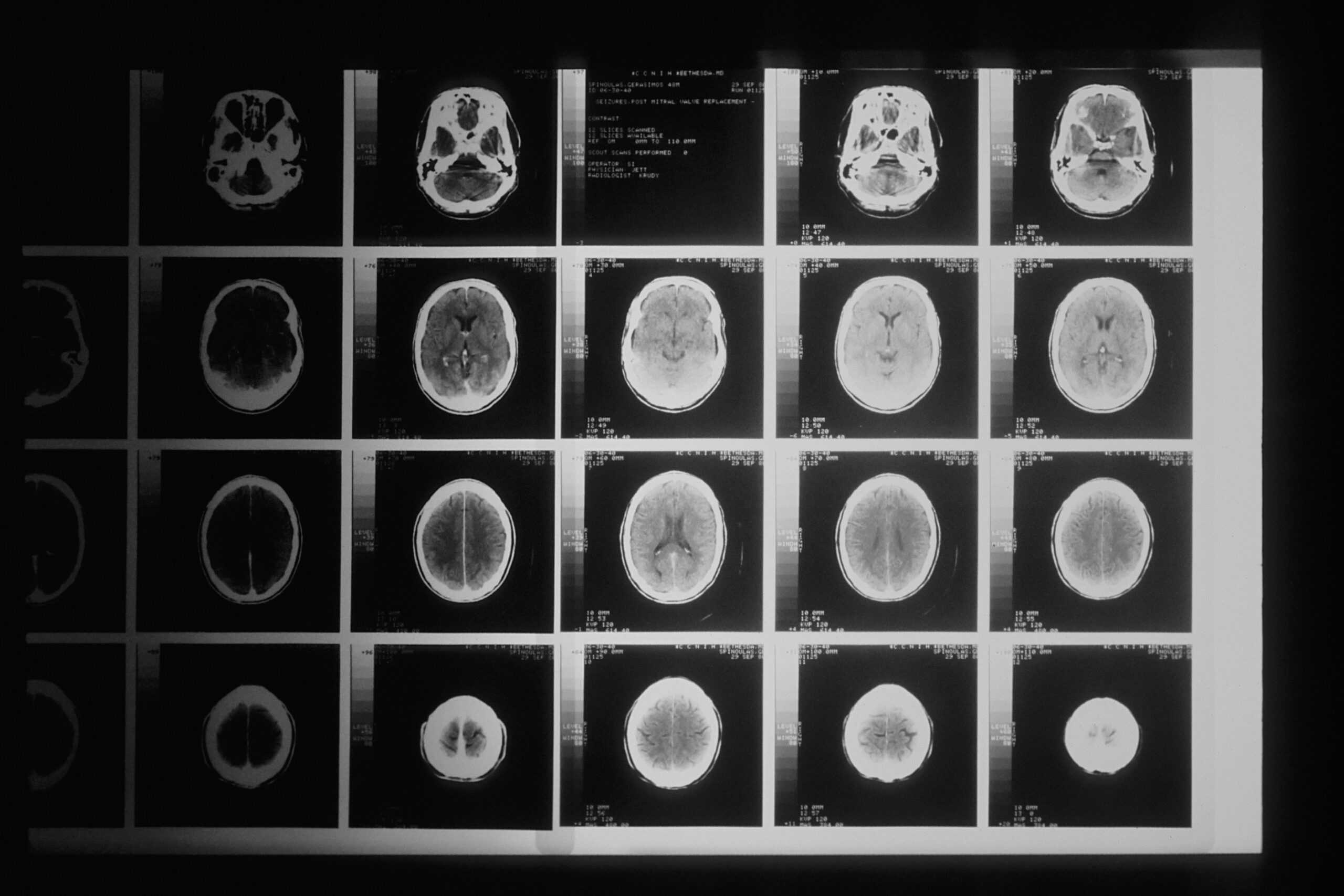
Thyroid Hormones and Cognitive Function
Delving into the thyroid-OCD connection involves recognizing that imbalances in thyroid hormones, crucial for regulating metabolism, can extend their influence to cognitive functions.
Hypothyroidism, characterized by low thyroid hormone levels, may contribute to difficulties in concentration and memory – facets closely tied to the cognitive aspects of OCD.
Assessing thyroid function can be pivotal in identifying and addressing these cognitive dimensions in the overall management of OCD.
Impact on Treatment Response
The influence of hormones on treatment response in OCD is a nuanced consideration. Hormonal variations may alter the metabolism and efficacy of medications commonly prescribed for OCD.
Additionally, hormonal fluctuations such as female reproductive cycle events may affect an individual’s responsiveness to cognitive-behavioral therapies.
Recognizing this intricate relationship aids clinicians in refining treatment plans, ensuring that interventions align with the individual’s hormonal profile for optimal therapeutic outcomes.
The Role of Neurotransmitters
Within the neurobiological context, hormones intricately interact with neurotransmitters, such as serotonin, dopamine, and norepinephrine.
Hormone imbalances can impact the synthesis, release, and reuptake of these neurotransmitters, influencing mood regulation and cognitive processes associated with OCD.
This dual influence underscores the importance of considering both hormonal and neurotransmitter dynamics in devising comprehensive treatment strategies.
The Mind – Body Connection and OCD
Thoughts and Triggers
At the core of OCD lies the interaction between distressing thoughts and ensuing compulsive behaviors. This symbiotic relationship is characterized by a profound mind-body connection.
An intrusive thought triggers a cascade of physiological responses – heightened anxiety, increased heart rate, and neuroendocrine alterations.
Recognizing these interconnected reactions elucidates the integral role of the mind in shaping the body’s response within the context of OCD.
Stress as a Catalyst
Stress serves as a catalytic force in the intricate correlation between mind and body in OCD. Elevated stress levels, originating from both internal and external sources, induce a physiological response.
For individuals contending with OCD, this heightened stress amplifies obsessive ideation and propels compulsive behaviors.
The discernment of stress as a key catalyst elucidates the profound relationship between psychological stressors and their somatic repercussions.
Neurotransmitters and Brain Chemistry
The neurobiological underpinnings of OCD bring forth the relevance of neurotransmitters and brain chemistry. The mind, as the locus of thoughts and emotions, communicates through these intricate chemical messengers.
Imbalances, particularly in serotonin, impact both mental and physical domains, contributing to the cyclical nature of obsessive thoughts and compulsive rituals.
Scrutinizing this mind-body nexus sheds light on the disruptions within brain chemistry that characterize OCD.
Physical Manifestations of Compulsions
Compulsive behaviors represent the tangible embodiment of the mind’s endeavor to mitigate distressing thoughts.
This aspect of the mind-body connection is evident in the repetitive actions undertaken to alleviate mental anguish.
Recognizing how the body actively participates in these coping mechanisms is essential to comprehending the cyclical reinforcement between mental distress and corresponding physical responses.
Impact of Behavioral Therapies
Behavioral therapeutic modalities, notably Exposure and Response Prevention (ERP), embody a professional approach that explicitly addresses the mind-body connection in OCD.
These interventions strategically engage both the cognitive and physiological facets by exposing individuals to distressing thoughts while inhibiting compulsive responses.
The efficacy of such therapies hinges on a comprehensive understanding of the intricate interplay between mental processes and physical manifestations.
In summation, the professional exploration of the mind-body connection in OCD is characterized by a recognition of the intricate dance between cognitive processes and physiological responses.
This understanding not only enriches our comprehension of the disorder but also informs therapeutic strategies aimed at fostering a holistic and efficacious approach to managing OCD.
Final Thoughts – Can Hormone Imbalance Cause OCD?
In conclusion, the question of whether hormone imbalance can cause Obsessive-Compulsive Disorder (OCD) unveils a nuanced and intricate connection between our physiological makeup and mental well-being.
Delving into this inquiry has provided valuable insights into the potential impact of hormonal fluctuations on the onset and modulation of OCD symptoms.
The recognition of stress hormones influencing OCD intensity, the role of reproductive hormones in symptom variation, and the intricate dance of thyroid hormones in cognitive function has broadened our understanding of the multifaceted relationship between hormones and OCD.
Moreover, acknowledging the impact of hormonal fluctuations on treatment response emphasizes the need for personalized approaches in managing OCD effectively.
As we navigate this exploration, it becomes clear that the link between hormone imbalance and OCD is not a one-size-fits-all scenario. Rather, it involves a complex interplay that extends beyond a simple cause-and-effect relationship.


