Mental Gymnastics: Navigating the OCD Cycle

In the world of Obsessive-Compulsive Disorder (OCD), individuals grapple with a recurring pattern of obsessive thoughts and compulsive behaviors.
Picture a mind caught in a loop of irrational fears, driving repetitive actions in search of relief. This is the challenge posed by the OCD cycle.
In this exploration, we delve into the mechanics of this cycle, its impact on daily life, and practical strategies to break free.
Join us as we unravel the complexities and empower individuals to regain control over their thoughts and behaviors.
What is the OCD Cycle
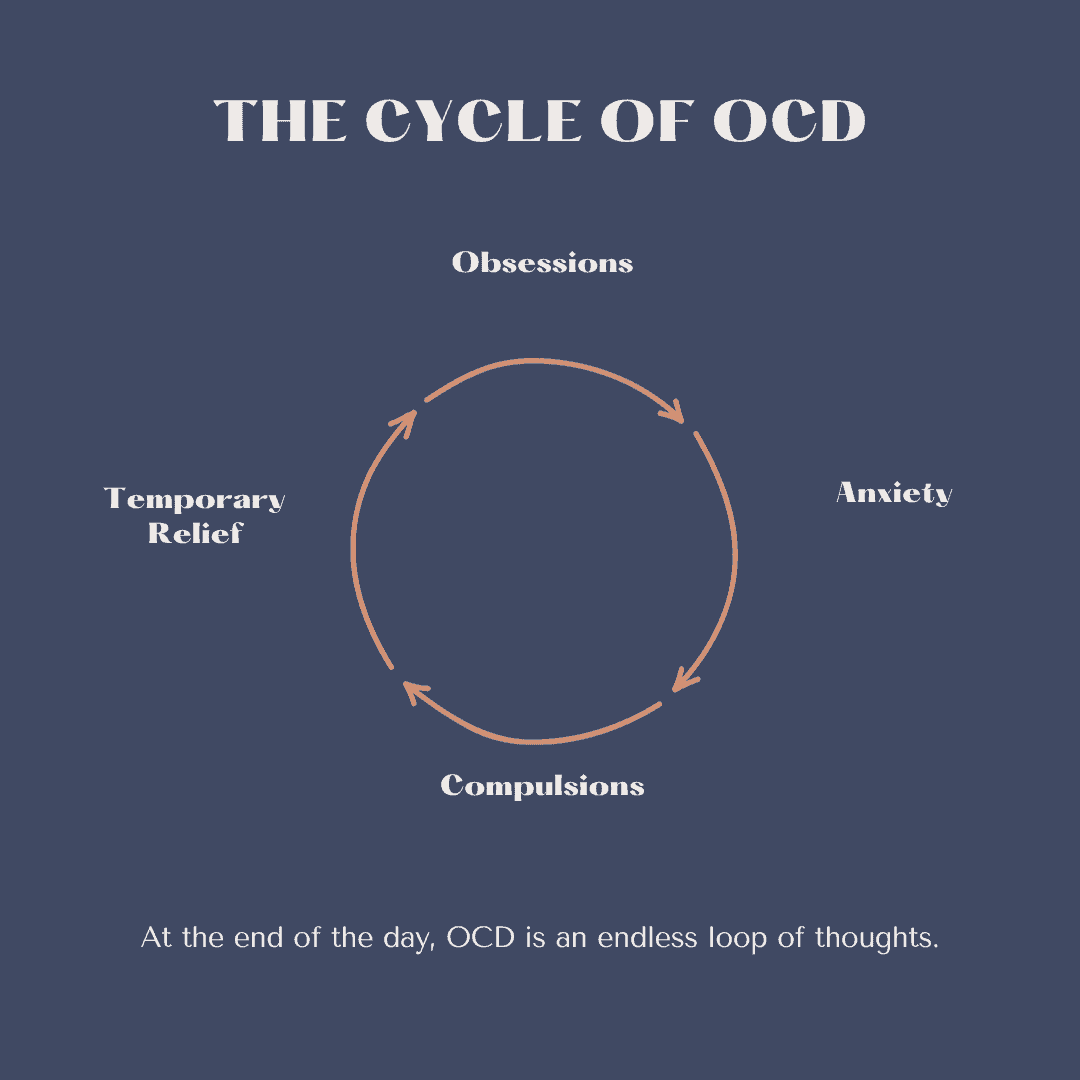
In the OCD cycle, individuals experience distressing obsessions, which are intrusive and unwanted thoughts, images, or urges. These obsessions trigger intense anxiety.
To cope with this anxiety, individuals engage in compulsions – repetitive behaviors or mental acts. Compulsions are aimed at preventing a feared event or reducing the distress associated with the obsession.
Despite the relief compulsions may temporarily provide, the anxiety tends to return, and the cycle repeats. Over time, individuals may find themselves trapped in this pattern, affecting their daily life and causing significant distress.
Treatment often involves cognitive-behavioral therapy (CBT), specifically exposure and response prevention, to help break the cycle.
Obsessions in the OCD Cycle
Obsessions in the OCD cycle encompass a wide range of distressing thoughts, fears, or mental images that are persistent and intrusive.
These obsessions or obsessive thinking patterns often center around themes like contamination, harm to oneself or others, fears of making a mistake, or concerns about order and symmetry.
The key characteristic is the distress these thoughts cause, leading individuals to attempt to neutralize or alleviate this distress through compulsive behaviors.
Common obsessions include worries about cleanliness, fears of harming others, doubts about safety, and concerns about moral or religious issues.
Despite being recognized as irrational, the obsessions generate significant anxiety, compelling individuals to engage in compulsive rituals as a way to regain a sense of control or prevent perceived harm. Understanding and addressing these obsessions is crucial in breaking the cycle of OCD.
Anxiety Caused By Obsessions
The anxiety caused by obsessions in the context of Obsessive Compulsive Disorder is multi-faceted, involving not only immediate emotional distress but also pervasive cognitive turmoil.
Individuals grappling with obsessive thoughts often experience a heightened sense of uncertainty and impending doom. The anxiety can infiltrate various aspects of their daily lives, impairing concentration, disrupting sleep, and affecting overall well-being.
Moreover, the obsessive thoughts often challenge fundamental beliefs or values, amplifying the emotional toll.
The fear and discomfort generated by these obsessions can create a constant undercurrent of unease, making it challenging for individuals to find respite from the distressing thoughts.
Recognizing the disproportionate nature of the anxiety and its irrational roots is a crucial step in therapeutic interventions designed to help individuals manage and eventually overcome OCD.
Compulsions in the OCD Cycle
Compulsions in the OCD cycle refer to the repetitive behaviors or mental rituals that individuals feel compelled to perform in response to their obsessive thinking patterns.
These actions are driven by a strong desire to reduce the anxiety triggered by intrusive thoughts or to prevent a feared event from occurring. Compulsive behavior often provide a temporary sense of relief, reinforcing the cycle, even though they are not connected to the actual threat.
Common compulsions include rituals related to cleanliness or contamination, checking behaviors to ensure safety, repeating actions until they feel “just right,” or seeking reassurance from others.
The compulsive behaviors are not connected logically to the feared event but serve as a means of attempting to gain control over the perceived threat.
Breaking free from the OCD cycle involves challenging and gradually reducing these compulsions through therapeutic interventions like exposure and response prevention.
Temporary Relief
The temporary relief individuals experience after engaging in compulsions in the context of Obsessive Compulsive Disorder (OCD) is a central aspect of the cycle.
Immediately following the ritualistic behavior, there is a transient sense of reduced anxiety and distress.
This relief serves as a powerful reinforcement mechanism, strengthening the association between the compulsive act and the alleviation of distressing feelings.
However, this relief is short-lived and illusory, as the underlying obsessions persist.
Over time, individuals often find themselves caught in a cycle of increasing compulsive behaviors, as the temporary relief becomes a compelling motivator to repeat the ritual whenever anxiety surfaces.
This reinforces the maladaptive coping mechanism, making it challenging to break free from the cycle.
Breaking the pattern involves resisting the urge to engage in compulsions and learning healthier ways to manage anxiety without relying on these repetitive actions.
How To Stop The OCD Cycle
Mindfulness and Relaxation Techniques:
Practice mindfulness meditation to increase awareness and acceptance of intrusive thoughts without judgment.
Learn relaxation techniques, such as deep breathing or progressive muscle relaxation, to manage anxiety caused by obsessive thoughts.
Exposure and Response Prevention (ERP):
Gradually expose yourself to situations that trigger obsessions, resisting the urge to perform compulsive behaviors.
Start with less distressing situations and progressively work towards more challenging ones.
Challenge Irrational Thoughts:
Identify and challenge distorted thoughts associated with obsessions. Ask yourself if your fears are based on realistic or irrational beliefs.
Create a Hierarchy:
Develop a hierarchy of anxiety-provoking situations, ranking them from least to most distressing. Gradually face each situation, moving up the hierarchy.
Mind-Body Connection:
Engage in regular physical activity to help manage stress and anxiety.
Ensure adequate sleep, as lack of sleep can exacerbate OCD symptoms.
Support System:
Share your struggles with trusted friends or family members. Having a support system can provide emotional assistance and understanding.
Professional Help:
Seek guidance from a mental health professional, preferably one experienced in treating OCD. Cognitive-behavioral therapy (CBT) with ERP is often the primary therapeutic approach.
Medication Management:
Consult with a psychiatrist about the potential benefits of medication, such as SSRIs, in managing OCD symptoms.
Educate Yourself:
Learn more about OCD to better understand the condition and its treatment options.
Remember, progress may be gradual, and it’s essential to be patient and persistent in implementing these strategies. If you’re struggling with any mental disorders, seeking the guidance of a mental health professional is crucial for personalized support and good or fair insight.
Effective Treatment

Cognitive-Behavioral Therapy (CBT):
Utilizes techniques such as Exposure and Response Prevention (ERP) to expose individuals to anxiety-provoking situations and prevent the accompanying compulsive behaviors. CBT also involves cognitive restructuring to challenge and change irrational intrusive thoughts.
Medication (Selective Serotonin Reuptake Inhibitors – SSRIs):
Antidepressant medications, particularly SSRIs like fluoxetine (Prozac), sertraline (Zoloft), or fluvoxamine, are often prescribed to help alleviate the symptoms of OCD by affecting serotonin levels in the brain.
Dialectical Behavior Therapy (DBT):
Incorporates mindfulness and acceptance strategies to enhance emotional regulation and interpersonal effectiveness, making it beneficial for managing intense emotions often associated with OCD.
Acceptance and Commitment Therapy (ACT):
Focuses on accepting unwanted thoughts and feelings without judgment and committing to actions in line with personal values. ACT aims to reduce the impact of obsessions on behavior.
Exposure and Response Prevention (ERP):
A specific form of CBT, ERP involves systematically exposing individuals to feared situations or thoughts while preventing the associated compulsive behaviors. This type of OCD treatment helps individuals learn to tolerate anxiety without resorting to rituals.
Habit Reversal Training (HRT):
Targets specific compulsive behaviors by identifying and replacing them with alternative responses. HRT is particularly useful for individuals with repetitive and ritualistic actions.
These therapies can be used alone or in combination, depending on the individual’s needs and preferences.
The effectiveness of treatment often depends on the severity of anxiety disorder symptoms and the willingness of the individual to actively participate in therapy.
It’s important to consult with mental health professionals and your mental healthcare provider to determine the most suitable therapeutic approach and an OCD diagnosis.
Final Thoughts on The OCD Cycle
In conclusion, breaking the OCD cycle is crucial for those with Obsessive-Compulsive Disorder.
Recognizing irrational thoughts, coupled with therapies like CBT and ERP, provides a foundation for recovery.
Incorporating mindfulness, acceptance techniques, and, when needed, medication, individuals can manage anxiety and regain control.
The journey is personalized, emphasizing patience and collaboration with professionals for a path toward resilience and well-being.