OCD In Children

Some things in the world do not make sense. At the top of the list is children suffering with mental diseases. It is really difficult for children to experience and explain what they are going through. It breaks my heart that many children are being diagnosed for mental health diseases every day. Unfortunately, obsessive – compulsive disorder in children has become common.
This post answers your questions regarding Obsessive Compulsive Disorder in children and what you as parents should do.
OCD and Children
Obsessive-Compulsive Disorder (OCD) is a mental health condition that can affect people of all ages, including children. OCD is characterized by the presence of obsessions and/or compulsions that cause significant distress and interfere with daily functioning.
Let’s explore OCD in children in more detail:
Obsessions
These are intrusive and unwanted thoughts, urges, or mental images that occur repeatedly and cause anxiety or distress. In children, common obsessions may include fears of contamination, harm coming to themselves or their loved ones, a need for symmetry or exactness, or excessive doubts.
Compulsions
Compulsions are repetitive behaviors or mental acts that individuals feel compelled to perform in response to their obsessions, often in an attempt to alleviate anxiety or prevent a feared event. Common compulsions in children include excessive handwashing, checking behaviors, counting, repeating certain words or phrases, arranging objects in a particular order, or seeking reassurance from caregivers.
Onset and prevalence
OCD can start during childhood, with the average age of onset being around 10-12 years. However, it can also manifest in younger children. OCD affects approximately 1-2% of children and adolescents, making it one of the most common psychiatric disorders in this age group.
Impact on daily life
OCD can significantly impact a child’s daily life, including their academic performance, relationships with peers and family members, and overall well-being. Children with OCD often spend a significant amount of time engaging in obsessions and compulsions, which can interfere with their ability to concentrate on schoolwork or participate in social activities.
Co-occurring conditions
Children with OCD may also experience other mental health conditions such as anxiety disorders, depression, attention-deficit/hyperactivity disorder (ADHD), or tic disorders. These conditions can further complicate the diagnosis and treatment of OCD.
Family involvement
It’s essential for parents and family members to be involved in the treatment process. They can provide support, encourage their child to engage in treatment, and learn strategies to manage OCD-related behaviors and reduce family accommodation (e.g., engaging in rituals to reduce the child’s anxiety).
Early identification and intervention are crucial in managing OCD in children. If you suspect your child may have OCD, it’s recommended to consult a mental health professional for a comprehensive evaluation and appropriate treatment options.
Causes Of OCD In Children
The exact cause of Obsessive-Compulsive Disorder (OCD) is not fully understood. However, researchers believe that a combination of genetic, neurological, environmental, and psychological factors contribute to the development of OCD in children.
Here are some potential factors that may play a role:
Genetic factors
There is evidence to suggest that OCD can run in families. Children with a close relative (such as a parent or sibling) who has OCD are at a higher risk of developing the disorder themselves. Certain genes or variations in genes may contribute to an individual’s susceptibility to OCD, although specific genes associated with OCD have not been identified conclusively.
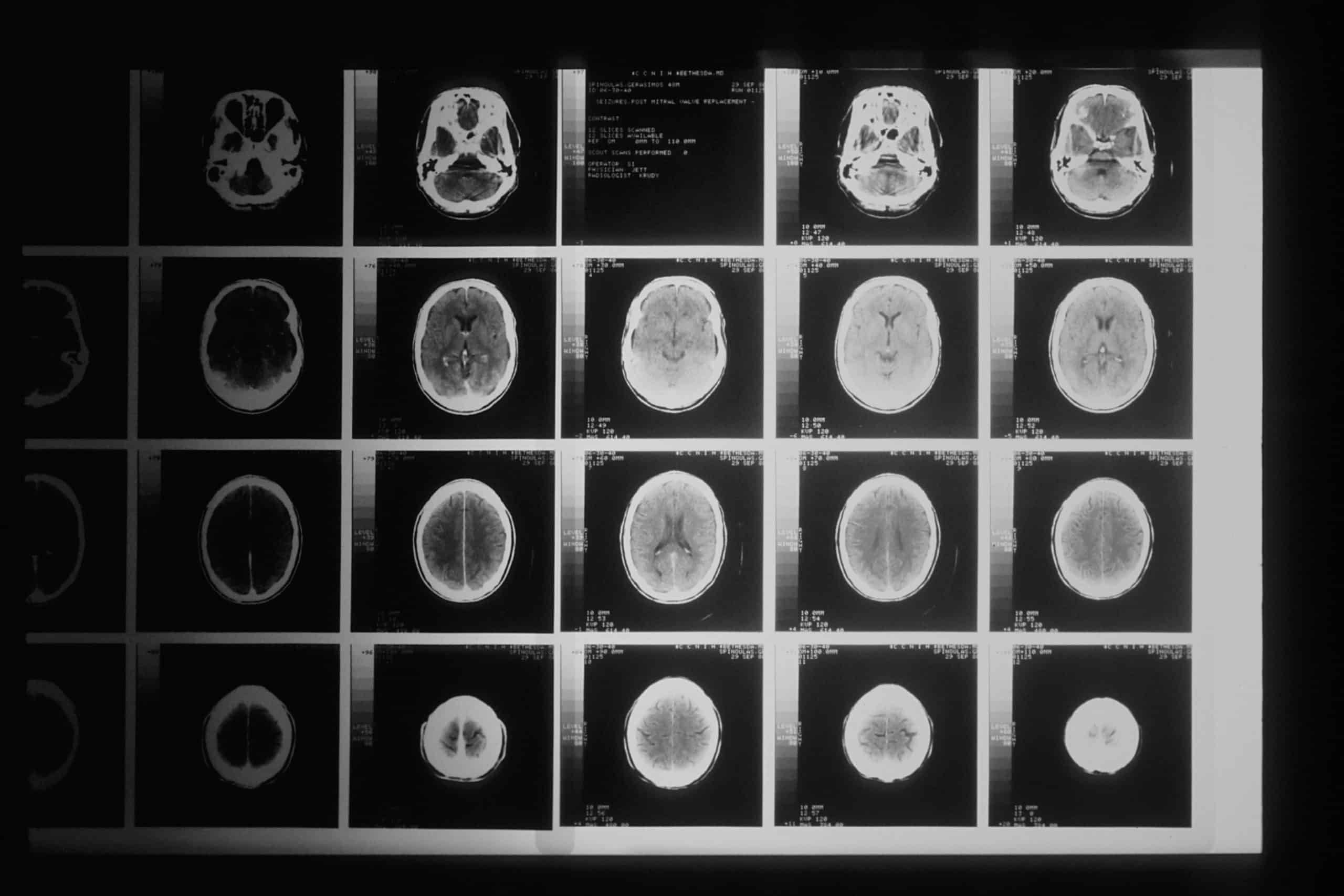
Neurobiological factors
Brain imaging studies have shown differences in brain structure and functioning in individuals with OCD. There may be abnormalities or dysregulation in certain areas of the brain, including the orbitofrontal cortex, anterior cingulate cortex, and basal ganglia, which are involved in decision-making, impulse control, and the regulation of anxiety.
Neurotransmitter imbalances
Imbalances in certain neurotransmitters, such as serotonin, dopamine, and glutamate, have been implicated in the development of OCD. These neurotransmitters play a role in regulating mood, anxiety, and impulse control.
Environmental factors
Some environmental factors may contribute to the development or exacerbation of OCD symptoms in children. Stressful life events, trauma, major life changes, or disruptions in family dynamics could potentially trigger or worsen OCD symptoms.
Cognitive factors
Certain cognitive factors, such as having a perfectionistic or excessively responsible personality, may increase the likelihood of developing OCD. Children who have a tendency to overestimate threats, have difficulty tolerating uncertainty, or have a heightened sense of personal responsibility may be more susceptible to OCD symptoms.
Behavioral conditioning
In some cases, the development of OCD symptoms can be influenced by learned behaviors. For example, a child may engage in a specific ritual or compulsion as a way to reduce anxiety or prevent a feared event. Over time, these behaviors can become reinforced and maintained, leading to the persistence of OCD symptoms.
It’s important to note that OCD is a complex disorder, and different factors may interact and contribute to its onset and maintenance in children. Additionally, not all children with these risk factors will develop OCD, and some children without apparent risk factors can develop the disorder. More research is needed to gain a deeper understanding of the causes of OCD in children.
How ocd is diagnosed in a child
Diagnosing Obsessive-Compulsive Disorder (OCD) in a child involves a comprehensive evaluation conducted by a mental health professional, such as a child psychiatrist or psychologist.
Here’s an overview of the diagnostic process for OCD in children:
Clinical Interview
The mental health professional will conduct a detailed interview with the child and their parents or caregivers. They will gather information about the child’s symptoms, their severity, duration, and impact on daily functioning. The interview may also explore the family history of OCD or other mental health conditions.
Diagnostic Criteria
The mental health professional will use the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association, to assess if the child’s symptoms meet the criteria for a diagnosis of OCD. The DSM-5 criteria include the presence of obsessions, compulsions, or both, causing significant distress or impairment.
Symptom Assessment
The mental health professional will evaluate the specific nature of the child’s obsessions and compulsions. They will assess the content, frequency, intensity, and duration of the symptoms to differentiate OCD from other mental health conditions with similar features.
Functional Impairment
The impact of OCD symptoms on the child’s daily life will be assessed. This includes evaluating how symptoms affect the child’s academic performance, social interactions, relationships, and overall functioning.
Differential Diagnosis
The mental health professional will rule out other possible explanations for the child’s symptoms. They will consider alternative diagnoses and determine if any co-occurring mental health conditions are present, such as anxiety disorders, depression, or tic disorders.
Parent/Caregiver Input
Parents or caregivers may be asked to provide additional information about the child’s symptoms, behavior patterns, and family dynamics. Their input can provide valuable insights into the child’s functioning at home and in different settings.
Duration and Course of Symptoms
The mental health professional will assess the duration of the child’s symptoms and any patterns of symptom onset, progression, or remission. This information helps in understanding the course of the disorder and planning appropriate treatment.
It’s important to consult a qualified mental health professional for an accurate diagnosis. They will consider the child’s unique circumstances, conduct a thorough evaluation, and provide appropriate recommendations for treatment and support.
How is ocd treated in a child

Obsessive-Compulsive Disorder (OCD) in children is typically treated using a combination of therapy and, in some cases, medication. The treatment approach aims to reduce symptoms, improve functioning, and enhance the child’s quality of life.
Here are the common treatment options for OCD in children:
Exposure and Response Prevention (ERP)
ERP is a highly effective form of CBT for OCD. It involves gradually exposing the child to their obsessive fears or triggers while preventing the accompanying compulsive behaviors. By resisting the urge to perform the compulsion, the child learns that their anxiety diminishes over time, leading to a reduction in symptoms.
Cognitive Restructuring
This component of CBT helps children identify and challenge irrational thoughts and beliefs that contribute to their OCD symptoms. The child learns to develop more realistic and balanced thinking patterns.
Skill-Building
Children learn various coping skills and techniques to manage anxiety, stress, and distress associated with OCD symptoms. They develop problem-solving skills and strategies to deal with triggers and difficult situations.
Selective Serotonin Reuptake Inhibitors (SSRIs)
These medications, such as fluoxetine (Prozac) or sertraline (Zoloft), are often prescribed for children with OCD. SSRIs help regulate neurotransmitters in the brain, which can reduce the frequency and intensity of OCD symptoms. Medication is usually used in combination with therapy, and the specific medication and dosage will be determined by a child psychiatrist.
Parent Education and Training
Parents are educated about OCD and its treatment, including understanding the disorder, learning techniques to support their child’s treatment, and reducing family accommodation (such as avoiding enabling compulsions or reassurance-seeking behaviors).
Family Therapy
Family therapy can help improve communication, reduce stress, and foster a supportive environment for the child’s recovery. It can also address any family dynamics or conflicts that may impact the child’s OCD symptoms.
Collaboration with School
Mental health professionals can work with the child’s school to create a supportive environment. This may involve providing information about OCD to teachers, implementing accommodations for academic needs, and addressing any social or educational challenges the child may face.
Treatment for OCD is highly individualized, and the specific approach will depend on the child’s unique needs and circumstances. Regular monitoring and follow-up with the treatment provider are essential to track progress and make adjustments as needed.
It’s important for parents and caregivers to seek help from qualified mental health professionals who specialize in treating pediatric OCD. Early intervention and consistent treatment can significantly improve the child’s prognosis and long-term outcomes.
How can I help my child live with OCD

Psychoeducation
- Teach your child about OCD: Explain the nature of OCD in age-appropriate terms. Help them understand that OCD is a medical condition and not their fault.
- Educate siblings and family members: Involve other family members in learning about OCD so they can offer support and understanding.
Encourage Expression
- Emphasize open communication: Create a safe and non-judgmental space for your child to express their feelings, fears, and concerns related to OCD.
- Validate their experiences: Let your child know that their feelings are valid and understandable, even if the obsessions and compulsions seem irrational to others.
Gradual Exposure
- Support exposure exercises: If your child is undergoing exposure therapy, work with their therapist to create a plan for gradual exposure to feared situations or triggers. Offer reassurance and encouragement during these exposures.
- Be a “brave buddy”: Accompany your child during exposures if appropriate, offering support and modeling bravery.
Implement Structure and Routines
- Create predictable routines: Establishing daily routines and schedules can provide a sense of control and security for your child.
- Set realistic expectations: Be understanding if OCD symptoms sometimes delay tasks or disrupt plans. Encourage your child to do their best while also recognizing their challenges.
Practice Mindfulness
- Teach mindfulness techniques: Help your child develop mindfulness skills to increase awareness of their thoughts and emotions. This can assist in managing anxiety and breaking the cycle of obsessive thoughts and compulsions.
Patience and Encouragement
- Celebrate progress: Acknowledge and celebrate even small victories and steps your child takes in managing their OCD symptoms.
- Patience during setbacks: Understand that setbacks may occur on the road to recovery. Offer support, reassurance, and patience during these times.
Peer Support
- Consider support groups: Look for local or online support groups for children with OCD and their families. Connecting with others facing similar challenges can provide a sense of community and understanding.
Self-Care for Parents
- Take care of yourself: Caring for a child with OCD can be demanding. Make sure you prioritize self-care, seek support from friends or support groups, and consider therapy for yourself if needed.
Remember, every child with OCD is unique, and what works for one child may not work for another. Stay attuned to your child’s individual needs, and collaborate with their treatment provider to develop a personalized approach for managing their OCD.
Final Thoughts On OCD and Children
In conclusion, supporting a child with OCD involves educating yourself and your child about the condition, creating a supportive environment at home, and actively participating in their treatment.
It’s important to encourage open communication, validate their experiences, and gradually expose them to feared situations with support. Implementing structure and routines, practicing mindfulness, and celebrating progress are essential.
Additionally, seeking peer support, advocating at school, and prioritizing self-care for both the child and parents contribute to a comprehensive approach in helping the child live with OCD successfully.