7 DBT Calming Techniques for OCD

In the journey of managing obsessive-compulsive disorder (OCD), individuals often seek comprehensive approaches that address not only the symptoms but also the underlying emotional and behavioral patterns contributing to their distress.
Dialectical Behavior Therapy (DBT) offers a unique framework that integrates mindfulness, acceptance, and skill-building techniques to empower individuals in their recovery.
In this guide, we explore how incorporating DBT calming techniques into existing OCD treatment can provide invaluable support, complementing traditional approaches with its emphasis on emotional regulation, distress tolerance, and self-awareness.
By understanding how to incorporate these techniques effectively and emphasizing consistency in practice, individuals can enhance their ability to cope with OCD symptoms and cultivate a greater sense of well-being.
What is Dialectical Behavior Therapy (DBT)?
Dialectical Behavioral Therapy (DBT) is a type of psychotherapy originally developed by psychologist Dr. Marsha Linehan in the late 1980s.
It was initially designed to treat individuals with borderline personality disorder (BPD) and other mental health conditions who often struggle with emotional dysregulation, impulsivity, interpersonal difficulties, and self-harming behaviors.
However, DBT has since been adapted to address a wide range of mental health conditions, including but not limited to depression, anxiety disorders, substance use disorders, eating disorders, and post-traumatic stress disorder (PTSD).
DBT is founded on the integration of several therapeutic approaches, including cognitive-behavioral techniques, mindfulness practices, dialectical philosophy, and acceptance-based strategies. Its primary goal is to help individuals build a life worth living by developing skills to manage intense emotions, emotional regulation skills, improve interpersonal relationships, and cope effectively with challenging situations.
The core principles of DBT include:
Dialectics
DBT is based on dialectical thinking, which emphasizes the acceptance of opposing truths and the synthesis of seemingly contradictory perspectives.
In therapy, this involves balancing acceptance and change, validation and change, and the dialectic between the therapist’s acceptance of the client as they are while also encouraging change.
Mindfulness
DBT incorporates mindfulness practices to help individuals become more aware of their thoughts, emotions, and sensations in the present moment without judgment.
Mindfulness skills teach individuals to observe their experiences without becoming overwhelmed by them, thus fostering greater self-awareness, emotional regulation and develop healthy coping skills for all type of mental health issues.
Distress Tolerance
DBT teaches skills to help individuals tolerate and cope with distressing situations without resorting to harmful or ineffective coping mechanisms.
This includes techniques such as distraction, self-soothing, and improving the moment to help individuals navigate crises without making impulsive or destructive decisions.
Emotion Regulation
OCD Dialectical Behavior Therapy (DBT) focuses on helping individuals identify, understand, and manage their emotions in healthy ways.
Emotion regulation skills include learning to recognize and label emotions, understanding the functions of emotions, and developing strategies to modulate emotional intensity.
Interpersonal Effectiveness
DBT teaches individuals skills to navigate interpersonal relationships effectively, assert their needs and boundaries, and communicate assertively. Interpersonal effectiveness skills help individuals build and maintain healthy relationships while reducing conflict and enhancing communication.
The goals of DBT include reducing problematic behaviors, improving emotional regulation, enhancing interpersonal functioning, and increasing overall quality of life.
Treatment typically involves a combination of individual therapy, interpersonal effectiveness techniques, skills training groups, phone coaching between sessions, and consultation for therapists to ensure adherence to the DBT model.
Overall, DBT offers a comprehensive and evidence-based approach to addressing the complex needs of individuals struggling with various mental health challenges, with a focus on building skills for a fulfilling and meaningful life.
How DBT Differs From Other OCD Treatments
Dialectical Behavior Therapy (DBT) offers a unique approach to treating obsessive-compulsive disorder (OCD) compared to other therapeutic modalities.
Here are some key ways in which DBT differs from other OCD treatments:
Incorporation of Mindfulness and Acceptance
DBT emphasizes mindfulness practices and acceptance-based strategies to help individuals with OCD develop a non-judgmental awareness of their obsessions and compulsions.
This approach encourages individuals to observe their thoughts and urges without becoming overwhelmed by them, fostering greater emotional regulation and reducing the need to engage in compulsive behaviors.
In contrast, traditional cognitive-behavioral therapy (CBT) for OCD typically focuses more on directly challenging and changing maladaptive thoughts and behaviors without as much emphasis on acceptance and mindfulness.
Focus on Emotion Regulation and Distress Tolerance
DBT places a significant emphasis on teaching emotion regulation and distress tolerance skills to help individuals cope with the intense emotions and distress often associated with OCD.
By learning to tolerate distress and regulate emotions more effectively, individuals can reduce the emotional reactivity that may exacerbate OCD symptoms.
While some other OCD treatments may touch on emotion regulation, DBT’s structured approach and specific skill-building exercises make it a central component of treatment.
Comprehensive Treatment Structure
DBT typically involves a structured treatment protocol that includes individual therapy, skills training groups, phone coaching between sessions, and consultation for therapists.
This comprehensive approach ensures that individuals receive support and guidance in various aspects of their recovery, including skill-building, application of skills in real-life situations, and ongoing support outside of therapy sessions.
While some other OCD treatments may include elements of skill-building or support, they may not offer the same level of structured, multi-component treatment as DBT.
Overall, DBT offers a unique and comprehensive approach to managing OCD symptoms by integrating mindfulness, acceptance, emotion regulation, and dialectical thinking into a structured treatment protocol. While other therapies may focus more narrowly on symptom reduction or behavioral change, DBT addresses the underlying emotional, cognitive, and interpersonal factors contributing to OCD in a holistic manner.
7 DBT Calming Techniques for OCD

Mindful Breathing
One of the core techniques in DBT is mindful breathing. This involves focusing attention on the breath, noticing the sensation of each inhale and exhale without judgment.
When individuals with OCD experience intrusive thoughts or urges to engage in compulsive behaviors, mindful breathing can help anchor them to the present moment, reducing anxiety and promoting a sense of calm.
By practicing mindful breathing regularly, individuals can cultivate greater awareness of their internal experiences and develop a tool for managing distressing thoughts and emotions.
Progressive Muscle Relaxation
Progressive muscle relaxation is a DBT skill that involves systematically tensing and then relaxing different muscle groups in the body. This technique helps individuals release physical tension and reduce overall arousal levels.
For individuals with OCD, who may experience heightened physiological arousal in response to obsessions and compulsions, progressive muscle relaxation can provide a sense of physical relief and relaxation. By learning to systematically relax the body, individuals can interrupt the cycle of tension and anxiety associated with OCD symptoms.
Wise Mind Acceptance
In DBT, “wise mind” refers to a state of balance between rational thinking and emotional experiencing. Wise mind acceptance involves acknowledging and validating one’s emotional experience while also recognizing the need for rational decision-making.
For individuals with OCD, who may struggle with intense emotions and the urge to engage in compulsive behaviors, wise mind acceptance can help them navigate difficult situations without being driven solely by emotion or impulse. By practicing wise mind acceptance, individuals can make more balanced and effective choices in managing their OCD symptoms.
Self-Soothe Activities
Self-soothe activities are DBT skills designed to provide comfort and relaxation in times of distress. These activities can include anything that engages the senses and brings a sense of pleasure or comfort, such as taking a warm bath, listening to calming music, or cuddling with a pet.
Grounding Techniques
Grounding techniques involve bringing attention to the present moment and anchoring oneself in reality. This can include focusing on sensory experiences, such as feeling the texture of an object, listening to ambient sounds, or noticing the sensation of feet on the ground.
Opposite Action
Opposite action is a DBT skill used to change emotions by acting opposite to the current emotion urge. For instance, if someone is feeling the urge to avoid a situation due to anxiety (a common experience for those with OCD), they might be encouraged to approach the situation instead.
Imagery-Based Relaxation
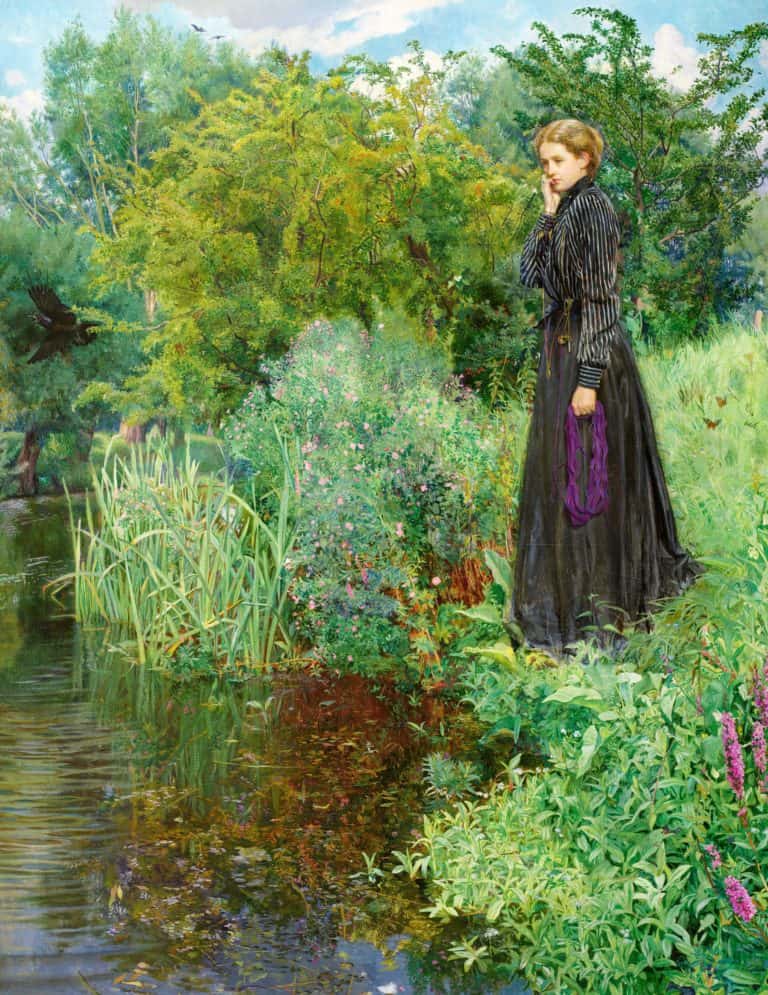
Imagery-based relaxation involves using guided imagery or visualization to evoke a sense of calm and relaxation. This technique can involve imagining oneself in a peaceful or serene setting, such as a beach or forest, and focusing on the sensory details of the scene.
How to Incorporate DBT Calming Techniques Into Your OCD Treatment

Incorporating Dialectical Behavior Therapy (DBT) calming techniques into your current OCD treatment can provide valuable additional tools for managing symptoms and enhancing overall well-being. Here’s how you can integrate DBT calming techniques into your treatment plan, emphasizing the importance of consistency:
Consult with Your Therapist
Start by discussing your interest in incorporating DBT calming techniques with a qualified mental health professional. They can provide guidance on which techniques may be most beneficial for your specific symptoms and circumstances. Your therapist can also help you develop a plan for integrating these techniques into your existing treatment regimen.
Identify Trigger Situations
Work with your therapist to identify situations or triggers that commonly exacerbate your OCD symptoms. This could include specific thoughts, feelings, or environmental cues that lead to increased anxiety or the urge to engage in compulsive behaviors. By recognizing these triggers, you can proactively apply DBT calming techniques when needed.
Practice Consistently
Consistency is key when it comes to incorporating DBT calming techniques into your OCD treatment. Set aside time each day to practice mindfulness, manage intense negative emotions, or other DBT skills. Consider integrating these techniques into your daily routine, such as practicing mindfulness during your morning routine or engaging in self-soothe activities before bed.
Use Techniques in Response to Obsessions and Compulsions
When you notice yourself experiencing obsessions or feeling the urge to engage in compulsive behaviors, apply DBT calming techniques to help manage distress and reduce anxiety. For example, use mindful breathing to ground yourself in the present moment, or practice opposite action by intentionally engaging in a calming activity instead of giving in to compulsions.
Final Thoughts on DBT Calming Techniques for OCD
In summary, integrating DBT calming techniques into your OCD treatment can complement existing strategies such as develop skills, healthy coping skills and provide positive emotional experiences. Consistency in practicing these techniques is essential for maximizing their effectiveness over time. By working closely with your therapist and committing to regular practice, you can enhance your coping skills and improve your overall quality of life despite the challenges of OCD (Obsessive compulsive disorder and other mental health condition(s).